At the time of writing, COVID-19 has taken the lives of over 33,000 people in the UK. The wrath of health inequalities in the UK is still prevalent during these times and rules the life expectancy outcomes of the poor. The death rate in deprived areas is twice as high as in richer areas.
People living in poorer areas are more likely to die of coronavirus because of a myriad of issues. These poorer areas are generally more densely populated with key workers (bus drivers, cleaners, nurses) unable to work from home and are therefore more likely to catch the virus. Social distancing is difficult in high rise flats with no gardens and with an added complication of using public transport to travel to work. The higher the density of population, the harder it is to be socially distant.
Those in low-incomes roles generally do not have the luxury of working from home compared to more affluent areas and careers and therefore put themselves at risk to simply earn a living.
People who live in poorer areas are also more likely to die from Covid because of pre-existing health conditions and have worse health than richer areas. This is due to lack of quality healthcare, higher stress levels, higher levels of poverty etc. It’s no surprise that because Salford is the 18th most deprived local authority and has 4 in 10 children living in poverty, that it has one of the highest Covid death rates outside of London.
The Inverse Care Law unfortunately is still present in the UK where the quality of healthcare is inversely related to the local health need i.e. deprived areas on average have worse health care than richer areas.
This shows the level of deprivation is directly linked to the death rates in the UK.

Covid deaths have also affected the BAME community with those from ethnic backgrounds twice as likely to die from the virus.

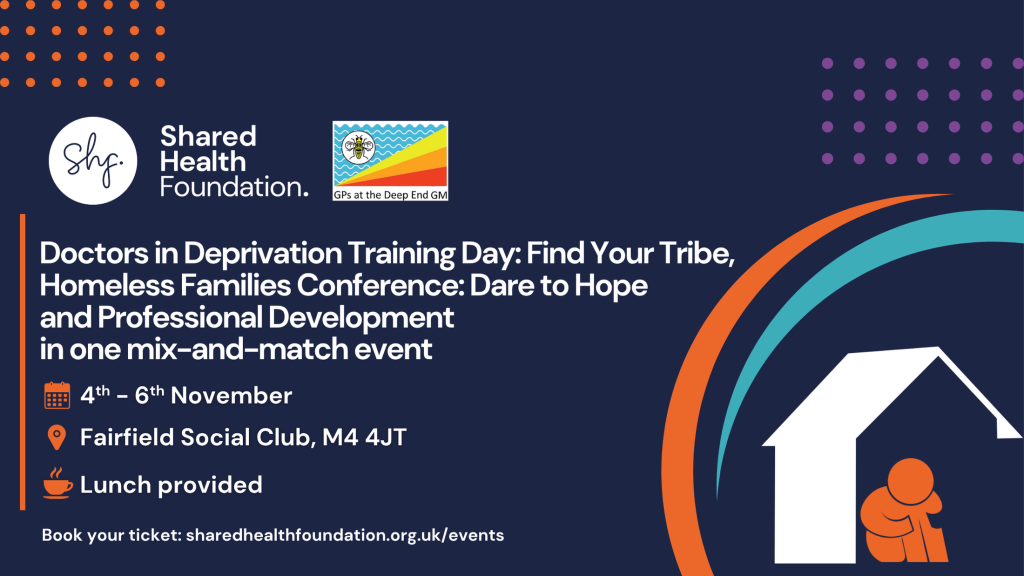
Health Inequalities in the UK is not a new story, nor will it disappear over night. Shared Health’s aim is to reduce the impact that poverty has on people’s health. Our work with Homeless Families, young people’s mental wellbeing, carers for under 7’s and GPs working in deprivation are needed now more than ever.
If the past 10 years of austerity have taught us anything, it’s that the poorest always get hit the hardest. That’s just not fair.
We are here to work at grassroots level to create new innovative projects and to work with councils to create policy change at regional and national level.
Contact@sharedhealth.org.uk